Min Addison
This blog is about me, my life and mostly about the rare disease called Addison disease.
Hund og Hoved imellem
Jeg skal nok få taget mig sammen, og skal lige have talt med hundetræneren om hun evt vil skrive lidt om det også. Men lige idag skal handle om mit mentale humør..

Et af mine store problemer med min sygdom, er at jeg ikke kan få en tanke til at blive til handling. Dvs jeg kan sidde her i stuen og tænke, jeg er tørstig og skal ud og hente noget at drikke.. men tanken kommer ikke videre og to timer senere sidder jeg stadig i stuen og tænker, jeg er tørstig..
Der kunne være ildebrand i mit hjem og jeg ville sidde og tænke, jeg skal ud herfra. men jeg ville blive siddende. Det er faktisk en meget skræmmende følelse, for man forstår jo godt at man skal lette sin po-po, man kan bare ikke. Kroppen forstår det ikke. Jeg tror kun det kan sammenlignes med hvis man er lam. Amerikanerne kalder det for en *brainfog*. det beskriver det faktisk ret godt..
Jeg har en ufattelig livsvilje, jeg nægter simpelthen at give op overfor denne sygdom. Hvorfor?
Tjow, det kan svares på meget enkelt.. Fordi jeg er en Mor.
Men man skal nok passe på med hvad man tror om noget man endnu ikke har prøvet. For det kan ikke undgåes at gå lidt ud over ham. Han er feks nødt til at tjekke med kammeraterne om de er sløje, før de får lov at komme her. Folk der er lidt sløje, er desværre ikke velkommen før de har det bedre, da en simpelt influenza, virus, forkølelse i sidste ende kan tage mit liv (men så er man altså også enormt udsat og uheldig).. Jeg skal helst holde mig fra syge og sløje mennesker.. Sjovt nok bliver jeg næsten aldrig smittet af Brian eller Frederik.. Måske det er fordi vi bor sammen og deler de samme bakterier.. Jeg aner det ikke.
Forrige år var Brian og Frederik på ferie på Mallorca, sammen med en kammerat. Jeg blev herhjemme. Jeg vidste godt at jeg ville være en hæmsko hvis jeg tog med, så jeg valgte at det var mere vigtig for mig at min søn fik en god aktiv (fysisk aktiv) ferie som han havde ønsket sig, med en masse minder om netop det han gerne ville opleve, fremfor hvis jeg var med så ville det meste være enormt stille og rolig og intet i stil med det han ønskede sig.
Han er den mest vidunderlige menneske jeg nogensinde har mødt.
Han er den dejligste ægtemand en kvinde kunne ønske sig og den mest fantastiske far, et barn kunne få.. Ham priser jeg mig lykkelig for hver eneste dag.
Idag har vi kendt hinanden i 18 år, så vi har nået endnu en milesten i vores liv. Planen er at om to år, fra dags dato, så skal vi have et kirkebryllup.. Vi er allerede borgerligt viet, men jeg vil enormt gerne give min Far den oplevelse at føre hans eneste datter op at kirkegulvet, og ja.. alt det andet der høre til et kirkebryllup.
Jeg er selv meget troende (på min egen måde) Brian er ikke troende og det har vi valgt at acceptere at på det punkt er vi forskellige og hvad Frederik vælger, skal være op til ham selv. Men i 2017 skal der holdes kirkebryllup. Så har jeg et nyt mål at nå..
Sidste år havde jeg valgt bare jeg kunne holde mig i live og oprejst til at komme gennem Frederiks konfirmation.. Da den var overstået stod jeg lidt og følte en vis tomhed, for hvad mål havde jeg nu.. Men mål er der nok af.. Jeg tager eet år af gangen, det bliver man nødt til med denne sygdom, Jeg kan ikke planlægge feks at skulle have hund om 5 år, for der er ikke garenti for jeg er her til den tid, så sådanne planer er kortfattede i min verden.
Jeg havde hørt at det var muligt at træne en hund til at reagere inden jeg blev syg.. Jeg vidste at det er muligt, fordi min gamle hunkat advarede mig når jeg var ved at blive syg. I starten forstod vi ikke hvad hun forsøgte at fortælle os, men som tiden gik, opdagede vi at hun fangede mine signaler inden jeg blev dårlig..
Hun var ikke en hyggenusse kat, hun ville gerne kæles og nusse, men kun på hendes præmisser. Når hun reagerede på mig, hang hun op af mig som et stykke gennemgnasket tyggegummi, sad på skødet af mig (selv når vi feks sad og spiste aftensmad), hun lå under min dyne i armen, miauved af mig konstant, puffede til mig, gik i vejen og man var slet ikke i tvivl om hun ville fortælle noget..
Desværre forlod hun os i en meget ung alder, hun var kun 6 år gammel da hun en aften kastede store mængder blod op. Hun blev hasteindlagt men afgik ved døden næste dags morgen.


Narnia → 
Nå.. men jeg fandt frem til at man kunne få en addison hund som kunne trænes netop til dette formål og det lød vildt spændende og lige noget for mig. Det var nok mere en drøm tror jeg, end at det rent faktisk kunne gå hen og blive virkelighed, var ikke så meget i mine tanker som selve tanke om at det var muligt.
Fenton skulle først tjekkes og godkendes af hundetrænerne, før jeg kunne få ham, men han bestod med bravour og flyttede ind hos os en fredag middag..




Fenton var vidunderlig.. Selv overfor kattene opførte han sig eksemplarisk og alt var faktisk lutter idyl, lige på nær mig (altså mit helbred).
Jeg havde simpethen ikke kræfter til at have en hvalp som var afhængig af mig. Det gik rimlig godt de andre dage, for der var Brian og Frederik der til at hjælpe mig, men da hverdagen begyndte med skole og arbejde og jeg skulle være alene hjemme med hund og helbred, samtidig med jeg pludselig satte 'noget andet' før min sygdom, der gik det galt.
Jeg er nødt til at ligge mig til at sove/hvile når jeg har brug for det, når min krop ber om det. Men har man en lille hvalp der står og tigger om at få lov at komme ud og gå en tur, så går man jo en tur. Det er logik.. Det måtte jeg indse at jeg ikke kunne på daværende tidspunkt, da jeg også var enormt dårlig gående og overanstregte min krop ufattelig meget.
Fenton nød at være 'på ferie' hos os. → 


Jeg SKAL have min Addison hund.. men der er enormt mange ting der skal falde på plads først, så vi ikke begår samme fejl som sidste gang. Det brænder dybt i min sjæl at jeg måtte opgive at have Fenton, han var en drøm at have, og ville have egnet sig enormt godt som servicehund.
Så jeg kæmper pt for at få mit hovede til at følge min krop, for hvor er det dog vidunderligt at jeg pludselig kan ting igen, jeg kan bare ikke overskue det endnu.. men jeg har troen på det kommer.
PS: Jeg kan kun anbefale denne Selyham Terrier som race til alle der ønsker en lille fantastisk klog, rolig og sjov hund. Især den mentale ro der er over racen, de er ikke vilde og voldsomme som mange terrier racer normalt er. Fentons stamnavn er Bussybuddy's Fenton og hans opdrætter Susanne bor på Fyn.
Fenton → 
Florinef
Dosage Form: Tablets
- Side Effects
- Dosage
- Professional
Florinef ® ACETATE
Fludrocortisone Acetate Tablets USP
Description
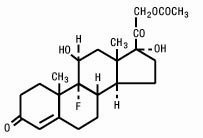
Florinef Acetate (Fludrocortisone Acetate Tablets USP) contains fludrocortisone acetate, a synthetic adrenocortical steroid possessing very potent mineralocorticoid properties and high glucocorticoid activity; it is used only for its mineralocorticoid effects. The chemical name for fludrocortisone acetate is 9-fluoro- 11ß,17,21-trihydroxypregn-4-ene-3,20-dione 21-acetate; its graphic formula is:
Florinef Acetate is available for oral administration as scored tablets providing 0.1 mg fludrocortisone acetate per tablet. Inactive ingredients: calcium phosphate, corn starch, lactose, magnesium stearate, sodium benzoate, and talc.
- Side Effects
- Dosage
- Professional
- Interactions
Clinical Pharmacology
Corticosteroids are thought to act, at least in part, by controlling the rate of synthesis of proteins. Although there are a number of instances in which the synthesis of specific proteins is known to be induced by corticosteroids, the links between the initial actions of the hormones and the final metabolic effects have not been completely elucidated.
The physiologic action of fludrocortisone acetate is similar to that of hydrocortisone. However, the effects of fludrocortisone acetate, particularly on electrolyte balance, but also on carbohydrate metabolism, are considerably heightened and prolonged. Mineralocorticoids act on the distal tubules of the kidney to enhance the reabsorption of sodium ions from the tubular fluid into the plasma; they increase the urinary excretion of both potassium and hydrogen ions. The consequence of these three primary effects together with similar actions on cation transport in other tissues appear to account for the entire spectrum of physiological activities that are characteristic of mineralocorticoids. In small oral doses, fludrocortisone acetate produces marked sodium retention and increased urinary potassium excretion. It also causes a rise in blood pressure, apparently because of these effects on electrolyte levels.
In larger doses, fludrocortisone acetate inhibits endogenous adrenal cortical secretion, thymic activity, and pituitary corticotropin excretion; promotes the deposition of liver glycogen; and, unless protein intake is adequate, induces negative nitrogen balance.
The approximate plasma half-life of fludrocortisone (fluorohydrocortisone) is 3.5 hours or more and the biological half-life is 18 to 36 hours.
Indications and Usage
Florinef Acetate is indicated as partial replacement therapy for primary and secondary adrenocortical insufficiency in Addison’s disease and for the treatment of salt-losing adrenogenital syndrome.
Contraindications
Corticosteroids are contraindicated in patients with systemic fungal infections and in those with a history of possible or known hypersensitivity to these agents.
BECAUSE OF ITS MARKED EFFECT ON SODIUM RETENTION, THE USE OF FLUDROCORTISONE ACETATE IN THE TREATMENT OF CONDITIONS OTHER THAN THOSE INDICATED HEREIN IS NOT ADVISED .
Corticosteroids may mask some signs of infection, and new infections may appear during their use. There may be decreased resistance and inability to localize infection when corticosteroids are used. If an infection occurs during fludrocortisone acetate therapy, it should be promptly controlled by suitable antimicrobial therapy.
Prolonged use of corticosteroids may produce posterior subcapsular cataracts, glaucoma with possible damage to the optic nerves, and may enhance the establishment of secondary ocular infections due to fungi or viruses.
Average and large doses of hydrocortisone or cortisone can cause elevation of blood pressure, salt and water retention, and increased excretion of potassium. These effects are less likely to occur with the synthetic derivatives except when used in large doses. However, since fludrocortisone acetate is a potent mineralocorticoid, both the dosage and salt intake should be carefully monitored in order to avoid the development of hypertension, edema, or weight gain. Periodic checking of serum electrolyte levels is advisable during prolonged therapy; dietary salt restriction and potassium supplementation may be necessary. All corticosteroids increase calcium excretion.
Patients should not be vaccinated against smallpox while on corticosteroid therapy. Other immunization procedures should not be undertaken in patients who are on corticosteroids, especially on high dose, because of possible hazards of neurological complications and a lack of antibody response.
The use of Florinef Acetate (Fludrocortisone Acetate Tablets USP) in patients with active tuberculosis should be restricted to those cases of fulminating or disseminated tuberculosis in which the corticosteroid is used for the management of the disease in conjunction with an appropriate antituberculous regimen. If corticosteroids are indicated in patients with latent tuberculosis or tuberculin reactivity, close observation is necessary since reactivation of the disease may occur. During prolonged corticosteroid therapy these patients should receive chemoprophylaxis.
Children who are on immunosuppressant drugs are more susceptible to infections than healthy children. Chicken pox and measles, for example, can have a more serious or even fatal course in children on immunosuppressant corticosteroids. In such children, or in adults who have not had these diseases, particular care should be taken to avoid exposure. If exposed, therapy with varicella zoster immune globulin (VZIG) or pooled intravenous immunoglobulin (IVIG), as appropriate, may be indicated. If chicken pox develops, treatment with antiviral agents may be considered.
Precautions
Adverse reactions to corticosteroids may be produced by too rapid withdrawal or by continued use of large doses.
To avoid drug-induced adrenal insufficiency, supportive dosage may be required in times of stress (such as trauma, surgery, or severe illness) both during treatment with fludrocortisone acetate and for a year afterwards.
There is an enhanced corticosteroid effect in patients with hypothyroidism and in those with cirrhosis.
Corticosteroids should be used cautiously in patients with ocular herpes simplex because of possible corneal perforation.
The lowest possible dose of corticosteroid should be used to control the condition being treated. A gradual reduction in dosage should be made when possible.
Psychic derangements may appear when corticosteroids areused. These may range from euphoria, insomnia, mood swings, personality changes, and severe depression to frank psychotic manifestations. Existing emotional instability or psychotic tendencies may also be aggravated by corticosteroids.
Aspirin should be used cautiously in conjunction with corticosteroids in patients with hypoprothrombinemia.
Corticosteroids should be used with caution in patients with nonspecific ulcerative colitis if there is a probability of impending perforation, abscess, or other pyogenic infection. Corticosteroids should also be used cautiously in patients with diverticulitis, fresh intestinal anastomoses, active or latent peptic ulcer, renal insufficiency, hypertension, osteoporosis, and myasthenia gravis.
Information for Patients
The physician should advise the patient to report any medical history of heart disease, high blood pressure, or kidney or liver disease and to report current use of any medicines to determine if these medicines might interact adversely with fludrocortisone acetate (see Drug Interactions ).
Patients who are on immunosuppressant doses of corticosteroids should be warned to avoid exposure to chicken pox or measles and, if exposed, to obtain medical advice.
The patient’s understanding of his steroid-dependent status and increased dosage requirement under widely variable conditions of stress is vital. Advise the patient to carry medical identification indicating his dependence on steroid medication and, if necessary, instruct him to carry an adequate supply of medication for use in emergencies.
Stress to the patient the importance of regular follow-up visits to check his progress and the need to promptly notify the physician of dizziness, severe or continuing headaches, swelling of feet or lower legs, or unusual weight gain.
Advise the patient to use the medicine only as directed, to take a missed dose as soon as possible, unless it is almost time for the next dose, and not to double the next dose.
Inform the patient to keep this medication and all drugs out of the reach of children.
Laboratory Tests
Patients should be monitored regularly for blood pressure determinations and serum electrolyte determinations (see WARNINGS ).
Drug Interactions
When administered concurrently, the following drugs may interact with adrenal corticosteroids.
Amphotericin B or potassium-depleting diuretics (benzothiadiazines and related drugs, ethacrynic acid and furosemide)—enhanced hypokalemia. Check serum potassium levels at frequent intervals; use potassium supplements if necessary (see WARNINGS ).
Digitalis glycosides —enhanced possibility of arrhythmias or digitalis toxicity associated with hypokalemia. Monitor serum potassium levels; use potassium supplements if necessary.
Oral anticoagulants —decreased prothrombin time response. Monitor prothrombin levels and adjust anticoagulant dosage accordingly.
Antidiabetic drugs (oral agents and insulin)—diminished antidiabetic effect. Monitor for symptoms of hyperglycemia; adjust dosage of antidiabetic drug upward if necessary.
Aspirin —increased ulcerogenic effect; decreased pharmacologic effect of aspirin. Rarely salicylate toxicity may occur in patients who discontinue steroids after concurrent high-dose aspirin therapy. Monitor salicylate levels or the therapeutic effect for which aspirin is given; adjust salicylate dosage accordingly if effect is altered (see PRECAUTIONS , General ).
Barbiturates, phenytoin, or rifampin —increased metabolic clearance of fludrocortisone acetate because of the induction of hepatic enzymes. Observe the patient for possible diminished effect of steroid andincrease the steroid dosage accordingly.
Anabolic steroids (particularly C-17 alkylated androgens such as oxymetholone, methandrostenolone, norethandrolone, and similar compounds)—enhanced tendency toward edema. Use caution when giving these drugs together, especially in patients with hepatic or cardiac disease.
Vaccines —neurological complications and lack of antibody response (see WARNINGS ).
Estrogen —increased levels of corticosteroid-binding globulin, thereby increasing the bound (inactive) fraction; this effect is at least balanced by decreased metabolism of corticosteroids. When estrogen therapy is initiated, a reduction in corticosteroid dosage may be required, and increased amounts may be required when estrogen is terminated.
Drug/Laboratory Test Interactions
Corticosteroids may affect the nitrobluetetrazolium test for bacterial infection and produce false-negative results.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Adequate studies have not been performed in animals to determine whether fludrocortisone acetate has carcinogenic or mutagenic activity or whether it affects fertility in males or females.
Adequate animal reproduction studies have not been conducted with fludrocortisone acetate. However, many corticosteroids have been shown to be teratogenic in laboratory animals at low doses. Teratogenicity of these agents in man has not been demonstrated. It is not known whether fludrocortisone acetate can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Fludrocortisone acetate should be given to a pregnant woman only if clearly needed.
Infants born of mothers who have received substantial doses of fludrocortisone acetate during pregnancy should be carefully observed for signs of hypoadrenalism.
Maternal treatment with corticosteroids should be carefully documented in the infant’s medical records to assist in follow up.
Nursing Mothers
Corticosteroids are found in the breast milk of lactating women receiving systemic therapy with these agents. Caution should be exercised when fludrocortisone acetate is administered to a nursing woman.
Pediatric Use
Safety and effectiveness in children have not been established.
Growth and development of infants and children on prolonged corticosteroid therapy should be carefully observed.
Geriatric Use
Elderly subjects may commonly have conditions that may be exacerbated by fludrocortisone therapy including, but not limited to, hypertension, edema, hypokalemia, congestive heart failure, cataracts, glaucoma, increased intraocular pressure, renal insufficiency, and osteoporisis (see WARNINGS , PRECAUTIONS and ADVERSE REACTIONS ). Elderly subjects may also commonly be taking concomitant drug therapy such as digitalis glycosides, oral anticoagulants, antidiabetic drugs (oral agents and insulin), and aspirin which may interact with fludrocortisone (see PRECAUTIONS - Drug Interactions ).
In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Adverse Reactions
Most adverse reactions are caused by the drug’s mineralocorticoid activity (retention of sodium and water) and include hypertension, edema, cardiac enlargement, congestive heart failure, potassium loss, and hypokalemic alkalosis.
When fludrocortisone is used in the small dosages recommended, the glucocorticoid side effects often seen with cortisone and its derivatives are not usually a problem; however the following untoward effects should be kept in mind, particularly when fludrocortisone is used over a prolonged period of time or in conjunction with cortisone or a similar glucocorticoid.
Musculoskeletal —muscle weakness, steroid myopathy, loss of muscle mass, osteoporosis, vertebral compression fractures, aseptic necrosis of femoral and humeral heads, pathologic fracture of long bones, and spontaneous fractures.
Gastrointestinal —peptic ulcer with possible perforation and hemorrhage, pancreatitis, abdominal distention, and ulcerative esophagitis.
Dermatologic —impaired wound healing, thin fragile skin, bruising, petechiae and ecchymoses, facial erythema, increased sweating, subcutaneous fat atrophy, purpura, striae, hyperpigmentation of the skin and nails, hirsutism, acneiform eruptions, and hives; reactions to skin tests may be suppressed.
Neurological —convulsions, increased intracranial pressure with papilledema (pseudotumor cerebri) usually after treatment, vertigo, headache, and severe mental disturbances.
Endocrine —menstrual irregularities; development of the cushingoid state; suppression of growth in children; secondary adrenocortical and pituitary unresponsiveness, particularly in times of stress (e.g., trauma, surgery, or illness); decreased carbohydrate tolerance; manifestations of latent diabetes mellitus; and increased requirements for insulin or oral hypoglycemic agents in diabetics.
Ophthalmic —posterior subcapsular cataracts, increased intraocular pressure, glaucoma, and exophthalmos.
Metabolic —hyperglycemia, glycosuria, and negative nitrogen balance due to protein catabolism.
Allergic Reactions —allergic skin rash, maculopapular rash, and urticaria.
Other adverse reactions that may occur following the administration of a corticosteroid are necrotizing angiitis, thrombophlebitis, aggravation or masking of infections, insomnia, syncopal episodes, and anaphylactoid reactions.
Overdosage
Development of hypertension, edema, hypokalemia, excessive increase in weight, and increase in heart size are signs of overdosage of fludrocortisone acetate. When these are noted, administration of the drug should be discontinued, after which the symptoms will usually subside within several days; subsequent treatment with fludrocortisone acetate should be with a reduced dose. Muscular weakness may develop due to excessive potassium loss and can be treated by administering a potassium supplement. Regular monitoring of blood pressure and serum electrolytes can help to prevent overdosage (see WARNINGS ).
Dosage and Administration
Dosage depends on the severity of the disease and the response of the patient. Patients should be continually monitored for signs that indicate dosage adjustment is necessary, such as remissions or exacerbations of the disease and stress (surgery, infection, trauma) (see WARNINGS and PRECAUTIONS , General ).
Addison’s Disease
In Addison’s disease, the combination of Florinef Acetate (Fludrocortisone Acetate Tablets USP) with a glucocorticoid such as hydrocortisone or cortisone provides substitution therapy approximating normal adrenal activity with minimal risks of unwanted effects.
The usual dose is 0.1 mg of Florinef Acetate daily, although dosage ranging from 0.1 mg three times a week to 0.2 mg daily has been employed. In the event transient hypertension develops as a consequence of therapy, the dose should be reduced to 0.05 mg daily. Florinef Acetate is preferably administered in conjunction with cortisone (10 mg to 37.5 mg daily in divided doses) or hydrocortisone (10 mg to 30 mg daily in divided doses).
Salt-Losing Adrenogenital Syndrome
The recommended dosage for treating the salt-losing adrenogenital syndrome is 0.1 mg to 0.2 mg of Florinef Acetate daily.
How Supplied
Florinef Acetate Tablets (Fludrocortisone Acetate Tablets USP), 0.1 mg/tablet: white, round, biconvex, scored tablets in bottles of 100 (NDC 61570-190-01); identification no. 429.
Store at room temperature; avoid excessive heat.
Prescribing Information as of July 2003.
Distributed by: Monarch Pharmaceuticals, Inc., Bristol, TN 37620
(A wholly owned subsidiary of King Pharmaceuticals, Inc.)
Manufactured by: Bristol-Myers Squibb Company, Princeton, NJ 08540 USA
fludrocortisone acetate tablet
More about Florinef (fludrocortisone)
Consumer resources
Professional resources
Related treatment guides
Drug Status
Availability Prescription only
CSA Schedule Not a controlled drug
Approval History Drug history at FDA
Drugs.com Mobile Apps
The easiest way to lookup drug information, identify pills, check interactions and set up your own personal medication records. Available for Android and iOS devices.
About
Terms & Privacy
Subscribe to receive email notifications whenever new articles are published.
Drugs.com provides accurate and independent information on more than 24,000 prescription drugs, over-the-counter medicines and natural products. This material is provided for educational purposes only and is not intended for medical advice, diagnosis or treatment. Data sources include Micromedex® (updated Jan 31st, 2018), Cerner Multum™ (updated Feb 2nd, 2018), Wolters Kluwer™ (updated Feb 2nd, 2018) and others. To view content sources and attributions, please refer to our editorial policy.
We comply with the HONcode standard for trustworthy health information - verify here
Addisons Syndrom
Hvad er addisons syndrom?
Addisons syndrom er en lidelse i binyrernes yderste lag, binyrebarken, der medfører nedsat eller ophørt produktion af livsvigtige hormoner som kortisol. Disse hormoner spiller en stor rolle for blandt andet opretholdelse af både sukker- og mineralstofskiftet.
Hvad er symptomerne på Addisons syndrom?
Binyrebark-hormonerne indvirker på de fleste af kroppens organer, og ved mangel på binyrebark-hormoner vil symptombilledet ofte være ganske varieret, men vil i typiske tilfælde kunne omfatte:
Hvordan kan din dyrlæge stille diagnosen?
Addisons syndrom er en af de lidelser, ders virkelig kan volde hovedbrud, når diagnosen skal stilles. Mistanken vil opstå ud fra de kliniske symptomer. Dyrlægen vil oftest udtage blodprøver for at få talværdier på indholdet af natrium, kalium og chlorid. Ændringerne af disse mineraler, især kalium, vil også kunne vise sig på en EKG- undersøgelse af hjertet. Den endelige diagnose baseres på en funktionstest på binyrerne, hvor der indgives et binyrestimulerende stof, hvorefter binyrernes respons herpå måles.
Hvordan behandles Addisons syndrom?
Behandlingen af Addisons syndrom vil være livslang tilførsel af binyrebarkhormon. Hvilken type af steroid dyrlægen vælger kan afhænge af om det hovedsageligt er mineral- eller sukkerstofskiftet der er påvirket af sygdommen. Langt de fleste patienter vil trives godt på den medicinske behandling.
Hvad er risikoen for at din hund for Addisons syndrom?
Sygdommen er sjælden og som før nævnt meget kompliceret, men efterhånden som stadig mere avancerede metoder til diagnostik vinder indpas, vil vi nok erkende flere tilfælde end tidligere.
Hvilke hunde er særlig udsatte for at få Addisons syndrom?
Sygdommen ses især hos unge til midaldrende tævehunde. Der mistænkes en arvelig disposition hos bl.a. Standard pudler i USA, men dette er endnu ikke fuldt afklaret.
af dyrlæger Henrik Strange og Kirsten Boeck Cushings syndrom er betegnelsen for et sygdomskompleks, der opstår, når organismen igennem længere tid udsættes for en øget mængde binyrebarkhormon. Disse …

Sunde, fedtfattige godbidder

Hundefoder til alle racer
Foder til sterilisterede/kastrerede hunde

Hundefoder til alle racer

Fuldfoder til voksne hunde

Fuldfoder til voksne mellemstore hunde

Vi sender faglig information, tips og tricks og gode tilbud 2-4 gange om måneden. Nye abonnenter får en rabatkode på 10% til webshoppen.


 Indhold på Netdyredoktor.dk
Indhold på Netdyredoktor.dk
Indholdet på Netdyredoktor.dk er udelukkende til informationsbrug. Disse informationer må på ingen måde kompensere eller erstatte den professionelle rådgivning og behandling, som gives af en autoriseret dyrlæge. Læs afsnittet om juridisk information og ansvarsfraskrivelse samt cookiepolitik .
Vores familiedyr er altid overladt til menneskers omsorg, både hvad angår pleje, sundhed og sygdom.
Det forpligter både dig som dyreejer og os som veterinærsygeplejersker og dyrlæger. Vi er med i et kompetent netværk, hvor vi altid kan trække på hinandens ekspertise. På den måde får dit dyr altid den bedste behandling.
Addison hund


Addisons sygdom hos hund

Hvad er Addisons sygdom?
Addisons sygdom er opkaldt efter Thomas Addison, som var den første, der demonstrerede at binyrerne er livsnødvendige. Binyrerne ligger i bughulen, ved siden af nyrerne, og det er derfor de kaldes for binyrerne. De producerer binyremarv- og binyrebarkhormoner. Hormoner er signalstoffer der produceres et sted i kroppen og transporteres med blodet til et andet sted i kroppen, hvor hormonet afkodes.
Addisons sygdom opstår, når binyrerne producerer for lidt binyrebarkhormon.
Hvorfor opstår Addisons sygdom?
Den hyppigste årsag til Addinsons sygdom, er at kroppens eget immunforsvar ødelægger binyrebarken. Kroppens immunforsvar angriber fremmede elementer som virus og bakterier, men af uvisse årsager kan det begynde at angribe kroppens egne celler. Immunsystemet ser altså cellerne i binyrerne som fremmede og angriber dem. Dette kalder man for en autoimmun sygdom.
Mindre almindelige årsager til Addisons sygdom er kræft eller infektioner i binyrerne. En overbehandling af Cushing´s syndrom, hvor kroppen producerer for meget binyrebark hormon, giver også Addisons sygdom.
Addisons sygdom er en relativt sjælden sygdom. Sygdommen er hyppigst hos yngre hunhunde, men angriber dog alle aldre og begge køn.
Hvad er symptomerne på Addisons sygdom?
Sygdommen kan opstå pludseligt, men vil oftest opstå langsomt over uger til måneder og være kronisk. Symptomerne er ikke specifikke, men nogle af følgende symptomer kan ses: ekstrem træthed, appetittab, opkastninger, diarré, vægttab, generaliseret svaghed og mental depression. Ved kronisk sygdom vil man se tilbagevendende perioder med maveproblemer i form af opkast og diarré og tiltagende træthed.
Hvordan stiller dyrlægen diagnosen?
Symptomerne på Addisons sygdom er meget uspecifikke. Mange andre sygdomme som hjerte-, lever-, nyre- og mavetarmsygdomme, giver samme symptomer, og er tilmed mere almindelige. Derfor vil dyrlægen ofte ikke mistænke Addisons sygdom som det første, og undersøge andre organsystemer inden Addisons sygdom bliver mistænkt. Når Addissons sygdom bliver mistænkt, kan en specifik test udføres for sygdommen. Testen der hyppigst bliver anvendt kaldes en ACTH stimulations test. Hvis testen er positiv kræves der livslang behandling.
Hvordan behandles Addisons sygdom?
Når diagnosen stilles vil hunden ofte have behov for intensiv behandling på et hospital. Når hunden kommer hjem skal den have binyrebarkhormon resten af livet, men vil kunne leve et normalt liv, når den rette dosis er fundet.


Seneste artikler












Mest læste
Hjerteorm
Hjerte- og karlidelser ![]() Dyrlæge Thea S. Kamstrup
Dyrlæge Thea S. Kamstrup
Hvad er hjerteorm? Fransk hjerteorm (Angiostrongylus vasorum) er en lille rundorm, der som voksen orm lever i hundens hjerte og blodkar. En hund smittet med Fransk hjerteorm kan få alvorlige hjerte-.
Skal jeg operere min hund med skedeprola…
Reproduktion ![]() Dyrlæge Thea S. Kamstrup
Dyrlæge Thea S. Kamstrup
Hej. Jeg har en hund på 8 år med en skedeprolaps, jeg har fået anbefalet at få den opereret og samtidigt steriliseret, er det virkeligt nødvendigt? er der ikke andre.
Mellemørebetændelse
Huden og øret ![]() Dyrlæge Thea S. Kamstrup
Dyrlæge Thea S. Kamstrup
Forekomst: ** Hvad er mellemørebetændelse? Øret deles traditionelt op i tre dele. Det ydre øre som består af øreflappen og den ydre øregang. Mellemøret som er et luftfyldt rum der er afgrænset.
Huden og øret ![]() Dyrlæge Thea S. Kamstrup
Dyrlæge Thea S. Kamstrup
Forekomst: *** Hvad er øremider? Øremiden Otodectes cynotis er et almindeligt problem hos killinger. Det er derimod væsentligt sjældnere at voksne katte smittes med øremider, og bliver de smittet får de voksne.
Huden og øret ![]() Dyrlæge Thea S. Kamstrup
Dyrlæge Thea S. Kamstrup
Forekomst: *** Hvad er øremider? Øremiden Otodectes cynotis er et relativt almindeligt problem hos hvalpe (killinger rammes dog væsentligt hyppigere end hvalpe). Det er sjældnere at voksne hunde smittes med øremider, og.
Leptospirose
Urin- og kønsorganer ![]() Dyrlæge Thea S. Kamstrup
Dyrlæge Thea S. Kamstrup
Under et skybrud, når vandmasserne overstiger kloakkernes kapacitet, kommer rotter og kloakvand op og blander sig med regnvandet. Ud over at kloakvand er uhygiejnisk og kan bære på mange smittekilder.
Sådan tjekker du hunden/katten for loppe…
Generelt ![]() Dyrlæge Thea S. Kamstrup
Dyrlæge Thea S. Kamstrup
Vi har desværre usædvanligt mange lopper i år, og lopper ser ud til at være et stadigt stigende problem. Så hvis du ikke behandler forbyggende mod lopper, er det en.
Hvorfor spiser hunde græs?
Fodring ![]() Dyrlæge Thea S. Kamstrup
Dyrlæge Thea S. Kamstrup
Hunde er i modsætningen til f.eks. katte, ikke strikte kødædere (carnivorer). Skal man forstå, hvorfor mange hunde synes om den ekstra ”snack”, skal man kigge på hundens forfader ulven, fra.
Grillmad kan være farligt for din hund
Fodring ![]() Dyrlæge Thea S. Kamstrup
Dyrlæge Thea S. Kamstrup
Der findes ikke meget mad der egner sig lige så godt til en lun sommeraften, som det der er tilberedt på en grill. Men det er ikke al grillmad, som.
Vidste du at hunde kan svede fra trædepuderne – men ikke på kroppen?
Ok, det er måske en sandhed med modifikationer. Der findes nemlig to typer af svedkirtler! Der findes de eccrine svedkirtler som giver en vandig sved, og det er denne type…
Min kat ryster på hoved
Min kat ryster meget på hovedet, som om den har noget i ørene. Når jeg ser ind i ørene ser de meget fine ud. Noget jeg kan gøre? Hilsen Ove Hej…
Min hund drikker og tisser meget
Hej Netdyrlæge Jeg har en lille Chihauhau. Den sover det meste af dagen. Begyndte at drikke meget og tisse meget. Så jeg troede den havde sukkersyge. Men nej, dens levertal var…
Rejse med kæledyr
For de senest opdaterede regler se Fødevarestyrelsens hjemmeside: http://www.foedevarestyrelsen.dk/Dyr/Rejse_med_kaeledyr/Sider/Rejse_med_kaeledyr.aspx
Vores schæfer er blevet aggressiv
Hej Thea. Jeg har skønne King på 5½ år, han er en hvid schæfer med lidt labrador i ;) For to år siden, blev han voldsomt angrebet af lopper og vi…
Forsikringsoversigt kat
Har du overvejet at tegne en sundhedsforsikring til din kat? Det kan være en god idé at gardere sig mod uforudsete dyrlægeregninger, ved at tegne en sundhedsforsikring. Der findes efterhånden flere…
Hvad er det for nogle knuder min kat har under maven?
Hej. Jeg har en dejlig stor rød hankat, han er 5 1/4 år og er meget glad og kælen. Han vil helst drikke frisk rindende vand fra vandhanen. Han får Hill's…
Min hund har store problemer med ørene - er det bedst hun får fred?
Hej Jeg har en dejlig hund, som jeg forguder, MEN som har øre problemer. Jeg har været ved dyrlæge med hende ca. hver anden måned, hvad gør jeg. Hun er ikke glad…
Hvordan hjælper jeg min hund med allergi?
Hej. Vi overtog sidste år en amerikansk cocker spaniel på knap to år. Vi fandt hurtigt ud af der var noget galt. Han gnavede poter, kløede ører og bagdel, og hans…
Min hund klør sig ved ørene, kan det være skab?
Hej, Min golden retriever 7 snart 8 år gammel har fået et hudproblem. Hun kom hjem med sår oppe på øret. Jeg behandlede det med Calendula og det helede op, men…
Ændret adfærd under falsk drægtighed
Hej Jeg har en 2 ½ år gammel Basset Fauve tæve. Indtil ca. 1 måned efter sidste løbetid har den været fuld af mod og krudt, og absolut ikke bange for…
Hvorfor slikker min hund på gulvet?
Min gamle hund er begyndt at slikke på gulvet – træ, marmor og hundekurv. Hvad tror du der er galt med den - eller hvad mangler den? Race: Jack Russel Køn: Han Alder:…
Problem: undervægt!
Hej Thea Problem undervægt! Medsendt stor blodprofil - ved udtagning havde hunden en smule øjenbetændelse, dette er behandlet - ligeledes blev der givet ormekur (der var ingen synlige orme hverken før…
Vores killing kan ikke holde balancen!
Vi købte 2 nye killinger for 4 uger siden, de 3 uger er gået godt i forhold til vores andre katte (2 hankatte og en hunkat), men så blev den…
Min kat har støvet pels og er slinger
Min kats pels ser ud som om den er støvet, og hun har fået det dårligere og dårligere indenfor de sidste 3 dage. Hun sover meget, spiser meget lidt, har…
- 1
- 2
- 3
- 4
- 5
Seneste om hund
Tilmeld dig nyhedsbrevet og vind gavekort på 500 kr.
I nyhedsbrevet kan du forvente at få nyheder,
Addison hund

Medikamente
Hier möchten wir kurz aufzeigen welche Medikamente Odin momentan in welcher Dosis bekommt. Nochmal betonen wir jedoch: Diese Angaben gelten ausschließlich für unseren Hund . Jedes Tier braucht eine auf es persönlich zugeschnittene Dosis.
Medikamente:
In der Anfangszeit wurde Odin alle 2 Wochen vom Tierarzt untersucht.
Durchgeführt wurde eine Blutkontrolle. Getestet wurden:
Wally Hund
Send Flowers Opens send flowers url in a new window
Guest Book
Not sure what to say?
May God bless you and your.
May your hearts soon be filled.
May the love of friends and.
As the days and weeks pass, and.
In loving memory of a wonderful.
Grief can be so hard, but our.
Get email updates about Wally Hund delivered directly to your inbox.
Just heard of the sad news, I'm so very shocked. Wally was a very dear friend, and he will be greatly missed. I'm so sorry we never had a reunion from St. Gertrudes or Leyden, he wanted to get that done. My sincere sympathy to his family. Love, Bunny
Mary Ann "Bunny" O'Donnell
August 20, 2005 | Franklin Park, IL
Dear Sharon and Family:
July 29, 2005 | Des Plaines, IL
We were very saddened to learn of your loss, and our being unable to join you at church. I will miss Wally. He was a unique person. I always enjoyed his company. Our sincere condolences to you.
Bruce and Melaine Pipkin
July 27, 2005 | Plainfield, IL
Dear Sharon and Family,
As you know, Wally treated me like a brother. For many years, we talked on the phone nearly every day, even though we lived 3000 miles apart.
He was an indefatigable bulldog, a pain in the neck and a first-rate friend. He accomplished much, but was most proud of his family and the legacy he created for you, your children and his grand children.
He was one in a billion and I already miss him.
July 25, 2005 | Newport Beach, CA
Beverly & Danny Quast
July 25, 2005 | FOX LAKE, WI
Heard of Wally's death while out of town.
July 25, 2005 | Elmhurst, IL
Our sympathy and prayers go out to the family of Mr. Wally Hund.
Nick & Musik Affatato
July 24, 2005 | Oak Brook, IL
Wally I will miss your great enthuiasim for the love of Golf, Rich Harvest Farm and Medinah, but most of all for the love of your entire family which you have always held First in your thoughts and heart. You were always there for all of us collectors who became to know you and were honored to be able to know you and call you, friend. To your Family and all of the Numerous friends we will now all have now a vast void in our hearts and souls, 'Till We Meet Again'.
July 24, 2005 | Pelham, NH
Sharon, Audrey and I were both saddened to hear of Wally's passing. His work on the Heritage of Medinah CC will always be appreciated. It was a work of Love for him. Our prayers are with you.
Bob & Audrey Rylowicz
Bob & Audrey Rylowicz
July 24, 2005 | Glen Ellyn, IL
Subscribe & Get Updates
Get email updates about Wally Hund delivered directly to your inbox.
Obituaries
Wally's Obituaries
Wally Hund, 65, of Addison, beloved and adored husband of Sharon; cherished father of Timothy (Christie), Jeff (Julie), Rick (Tami), Michelle (Brian) Stefan and Danny Hund; revered grandfather of Keith, Matthew, Ashley, Nicholas, Zachery, Kevin, Alexandria, Jeffery ''JJ'', Jillian, Justine.
Read Full Obituary
Add a Photo or Video
Advice & Support
Losing a loved one and coping with grief can be difficult. Let us help.
Addison's Disease in Dogs - Diagnosing, and Treating Hypothroidism
Dr. Michael Richards
Michael Richards, D.V.M. co-owns a small animal general veterinary practice in rural tidewater.
Michael Richards, D.V.M. co-owns a small animal general veterinary practice in rural tidewater Virginia. Dr. Richards graduated from Iowa State University's College of Veterinary Medicine in 1979, and has been in private practice ever since. Dr. Richards has been the director of the PetCare Forum.
Michael Richards, D.V.M. co-owns a small animal general veterinary practice in rural tidewater Virginia. Dr. Richards graduated from Iowa State University's College of Veterinary Medicine in 1979, and has been in private practice ever since. Dr. Richards has been the director of the PetCare Forum.
Question: I have a Dalmatian with Addison's disease. She gets a shot of percoten once a month and is doing very well. The cost of her shot has just gone up to $115.00 a month. Is there any way I can get this medication on my own and administer it? I am disabled and the expense is getting to be a real problem for me. The idea of putting her down is very disturbing to me especially since she has done so well with the treatment. Thank you, Irene
It may be a lot less expensive to treat with fludrocortisone IF you are willing to use a compounding pharmacy to obtain the medication and can afford to pay for some additional testing early on to make sure it works OK for your dog (monitoring potassium and sodium for a few weeks). There have been reports of compounded fludrocortisone not working as well but it is a lot less expensive and it appears to work for many dogs. You might ask your vet to check into this option for you, especially since the lower long term cost seems potentially critical to your Dalmatian's survival in your situation.
I do not know of any way that you could obtain Percorten-V legally for administration yourself in the U.S. Florinef (Rx), the brand name version of fludrocortisone is usually more expensive than Percorten-V for large dogs so it is unlikely that a change from one brand name to the other will be helpful.
There are a number of veterinary compounding pharmacies and many communities have a compounding pharmacy in them (ours does) that usually will work with veterinarians.
Mike Richards, DVM
Diagnosing hyperadrenocorticism (Cushing's) and hypothyroidism (Addison's)
I am a new subscriber and have been reading your ques/answers for a couple of weeks now. I am really impressed with the personal and in-depth information you provide. We have a twelve and a half year old pet, half German Shepherd half Golden Retriever, Princey by name. Princey has always been healthy with few health problems. Since the last few months, he has been drinking and urinating excessively. He has become almost completely bald at the collar area and has lost a lot of hair around his stomach area and a patch on his back, a little above his tail. His skin is dry and flaky, like dandruff. On the back area, near his tail where he has lost hair he has little raised bumps. We took him to his regular vet a few times but he said it was just old age, he took some x-rays as Princey's back legs seem to be bothering him, it takes him longer to get up. X-Rays showed slight arthritis. Around the middle of March, he was given steroids for two weeks and an aspirin a day. He finished his course of steroids and was on aspirin until April 20th. We have given him aspirin only twice after that. I don't like to put him on any medication until I am sure it is necessary and will not harm him but at the same time want to make sure he gets whatever he needs to get better. After reading your columns, we took Princey to a different vet on May 7th, as I was afraid Princey showed all the classic signs of Cushings. The new vet who seems to know a lot about Cushings, unlike the first one, examined Princey and did a urine and blood test. The urine test had a reading of one, which she said was very dilute but showed no trace of diabetes. The blood test, the vet said shows no sign of Cushings, she has asked we do a water deprivation test to rule out diabetes insipidus. She also said his thyroid levels are low and that could be causing the hair loss and skin problems and that we could put him on a thyroid supplement if his hair loss is bothering us but that it is not absolutely necessary at his age. Your column says though that sometimes blood tests are inconclusive for cushings. Also, will it hurt to put him on thyroxine if that really is not the problem? Does it have any side effects? Will it aggravate any other condition he might have, like Cushings or diabetes insipidus? Do you think we should push for more testing to rule out cushings? Is there any kind of skin test we can do? Dr. advised us to put aloe on his skin. His blood test results were all within the normal range except for these -
neutrophils 84 (normal 60 - 77),
lymphocytes 6 (normal 12 - 30),
lymphocytes absolute 570 (normal 690 - 4500),
alk phos 199 (normal 5 - 131),
GGT 24 (normal 1 - 12),
cholesterol 360 (normal 92 - 324),
BUN 10 (normal 6 -25),
creatinine 0.5 (normal 0.5 - 1.6),
BUN/Creat ratio 20 (normal 4 -27),
T4 RIA 0.42 (normal 1.0 - 4.0),
FREE T4 (RIA) 0.38 (normal 0.65 - 3.00),
uantitative platelets 448 (normal 70 - 400).
His AST(SGOT) was 29 and ALT (SGPT) was 70. The vet said his results were all okay for his age and that if he had cushings his alk phos levels would be markedly higher. Any input from you will be greatly appreciated as I am very worried about Princey and would like to get him back to his old self as soon as possible.
Thank you, padma
There are a lot of things to consider with the information that you have so far.
It is not possible to diagnose hyperadrenocorticism (Cushing's disease) based on the results of a standard blood chemistry examination nor is it possible to rule it out based on these results. It is true that many dogs with Cushing's disease have elevations in the alkaline phosphatase levels in their serum, but many do not, as well. It is necessary to do some sort of specific testing in order to try to rule in or rule out the Cushing's disease. The most commonly recommended test is a low dose dexamethasone suppression test (LDDS). This test takes most of a day to run. A blood sample is drawn early in the morning and immediately afterwards dexamethasone is administered intravenously. In four hours a second blood sample is drawn and after 8 hours a third blood sample is drawn. The cortisol levels of the samples are compared. If Cushing's disease is not present, the cortisol levels should go from normal levels to very low levels (they are suppressed). If Cushing's is not present, the cortisol levels remain high after the injection of the dexamethasone. An alternate test is the ACTH response test. This test is less sensitive to the presence of Cushing's disease but can be run much more quickly, making it more convenient at times. To do an ACTH response test, a blood sample is drawn any time during the day and then a hormone, adrenocorticotropin (ACTH) is administered. An hour later (two for some ACTH preparations) a second blood sample is drawn. If the results of the second sample show markedly elevated levels of cortisol, it indicates that Cushing's disease is present. There are other tests that help to determine what type of Cushing's disease is present but one of these two tests is a good idea to determine if Cushing's disease is present.
It is pretty important to know if Cushing's disease is present, prior to trying to decide if hypothyroidism is actually present. The reason for this is that the presence of almost any other disease can cause the thyroid levels in the blood stream to drop. Therefore, it is hard to test accurately for hypothyroidism in a patient who has a problem like Cushing's disease. If Cushing's disease is present and can be treated for, then it is possible to more accurately test for hypothyroidism. In some cases, especially when there is only a partial response to treatment for Cushing's disease, it may be necessary to go ahead and treat for hypothyroidism without being certain if it is present. Fortunately, it is relatively safe to supplement thyroxine in a dog, even if they don't actually have hypothyroidism. It is better to work to be sure that a life long supplement is necessary before giving it, whenever possible, though. Hypothyroidism can cause increased drinking and increased urination in some patients and the hair loss can also occur with either disease, so it is entirely possible it is present and that it is the sole problem, but increased drinking and urinating are much more common with hyperadrenocorticism.
I sometimes have a hard time asking a patient to spend money on Cushing's disease tests because in our practice, I am pretty sure that of the dogs I test, only about 25% of them actually have Cushing's disease and the tests only help determine one thing -- if Cushing's disease is present or not. However, since there isn't any other way to determine if the disease is present and since it is important to both the dogs that have it and those that don't to know what is going on, I know that it is necessary to do the testing. I really do think that I would want to know if Cushing's disease was present with the clinical symptoms that Princey has. So I do recommend asking your vet about futher testing.
Good luck with this.
Mike Richards, DVM
Addison's disease or Heat stroke death
Question: One of my questions relates to a 2 year old mastiff that I lost recently. He died within 24 hours of being at a kennel (1st time I had my dogs at a kennel). The autopsy said he died of heat stroke. His body temp. when the vet arrived at the kennel was 109 degrees. The kennel employees were not there when the dog collapsed and suspect that he may have been down for about 5 m in. The kennel also admitted that they were dumb-founded when it occurred and hesistated to call the vet and instead called our housesitter and our manager at our business to see if he had a preexisting condition. The reason I mention this is because they said it probably took about 25 min for them to administer 1st aid to my dog. They are claiming that although it was a very hot and humid day, they did not have my dog outside that long for him to have a heat stroke. The vet tech who arrived at the kennel stated that it was very warm inside the kennel also. I guess I'm trying to learn more about heat stroke to make sense of this. I looked up on the internet and it mostly talks about dogs being kept in cars. Could mastiff's be more susceptable to heat stroke? Also, our dogs are not kept outside and are exercised during cooler temp versus exposing them to extreme heat. Zeus was on Metronidazole , 500mg., for an upset stomach the week prior to his death. The autopsy showed that Zeus was in excellent health and his organs were normal. They did note that his adrenal glands were smaller than expected for his dog's size. His behavior prior to his death on that date according to the kennel that he was playing happily with our 2 other dogs, had a good appetite, and seemed to be happy as indicated by his tail wagging and affection. My particular quesitons are: 1) HOw long does it take for a dog's temp to reach 109 degrees (at the vet the week before his temp was normal). 2) HOw soon should a dog be cooled down when collapsing? Could cooling him down saved his life? 3) Could the medication predispose him to a heat stroke (he took the doses recommended and was off it already for 2days). 4) Did his smaller adrenal glands cause him to have a heat stroke?-- I apologize for asking questions that may not have exact answers. I'm trying to learn as much as I can so to further prevent another death and to educate myself about dog safety. I also need closure to my buddies death and hope time and more information may help. Thank your for your time and invaluable service. Angela
There are two strong possibilities with the situation you describe. The first one is that your dog simply had heat stroke and that all symptoms and his death were related to that. The second is that he had hypoadrenocorticism, or Addison's disease, which can lead to sudden death without any other predisposing cause and also makes almost any other stressful condition much worse. So I'm going to divide this answer into two parts, one to cover the heat stroke and one to cover the Addison's disease to some extent.
Heat stroke in dogs is not all that uncommon. Dogs do not have an efficient method of handling heat stress because they don't sweat and they don't seem to figure out that they shouldn't get excited or work hard in the heat, either. Heat stroke is most common in the large breeds and in dogs with short noses, so mastiffs are in the group of dogs that are most susceptible to this problem.
Death from heat stroke can occur pretty quickly. The shortest interval between exposure to high heat extremes and death is about 20 minutes, based on our practice experience, but these have been "closed car" cases. It is probably more common for dogs to experience heat stroke in the first few days they are acclimating to heat and for it to occur in conjunction with excitement or exercise. Most dogs probably take an hour or more to develop heat stroke in these circumstances but if they were struggling with the heat prior to exercising it is possible that the problem could develop more quickly. Any illness that is contributing to an increase in body temperature can also shorten the time period for signs to become severe.
The most common clinical signs of heat stroke are weakness, loss of balance, excessive panting, roaring breathing sounds, excessive salivation, decrease in mental awareness, collapse and death. Any time that heat stroke is suspected it is best to get an immediate rectal temperature reading and to begin treatment immediately if the body temperature is over 106 degrees Fahrenheit or to stop all activity and move indoors if the temperature is less than this but elevated above 103.0 degrees Fahrenheit. Body temperatures over 107 degrees Fahrenheit are a critical emergency, because organ damage can occur at this temperature and at higher temperatures.
Treatment consists of cool water (not cold water) bathes or rinses. If the water is too cold, or if ice is used to cool a heat stroke victim it can cause a decrease or loss of skin circulation, which can delay cooling. This should be done immediately for a few minutes and then the dog should be taken to the veterinarian's office or to an emergency veterinary clinic immediately. Most dogs will not drink water at this stage of heat stroke and it is not a good idea to spend time trying to get them to. Just go to the vet's as quickly as possible. The veterinarian may want to use cool water enemas, cool water gastric lavage (rinsing of the stomach), corticosteroids and specialized intravenous fluid therapy using colloids to maintain blood pressure. If there is any evidence of disseminated intravascular coagulation (DIC), intensive therapy for several days may be necessary if a successful outcome is possible.
Immediate treatment is critical to success when dealing with heat stroke, so delays are potentially harmful, or fatal. Many people do not associate the clinical signs they are seeing with heat stroke, though. Especially when their level of suspicion is not high. We have seen heat stroke in dogs who were swimming or who were merely excited but not obviously exercising hard, situations in which people often do not make an association with heat stroke. We have even had one bulldog patient who developed heat stroke in the house, with the air conditioning on, apparently because he became very excited about guests at the house for a party.
So heat stroke could easily be the whole problem.
On the other hand, small adrenal glands can be a sign of hypoadrenocorticism, or Addison's disease. In this disease there is a deficiency in the production of corticosteroids and mineralocorticoids (regulate electrolytes in the body). Patients with Addison's disease often have very vague signs of illness that is often chronic. Often these signs are vague enough that owners don't recognize them or don't seek treatment for them. The range of signs is large, but includes intermittent decreases in appetite, or dogs with a generally poor appetite, vomiting, diarrhea, muscular weakness, depression or lethargy, slow heart rates, increased drinking and urinating, cardiac arrhythmias, unexplained shock and sudden death. Most patients probably only have one or two of these signs at any given time and will never develop all of them.
Patients who respond poorly to stressful situations and especially patients who die from stress that most patients have no trouble handling are likely candidates for Addison's disease. It is likely that most veterinary patients with Addison's disease are diagnosed by accident when blood is drawn for other reasons or have their Addison's disease diagnosed only after a poor response to a stressful situation, such as their first surgery or a traumatic incident. Unfortunately, if they do progress to severe shock or death quickly, the diagnosis may not come in time.
I know of no link between the use of metronidazole and heat stroke, except that metronidazole can cause vomiting or diarrhea and any amount of dehydration induced by these conditions would lead to an increased possibility of heat stroke. I have not heard of any problems with the use of metronidazole in patients with Addison's disease. Overdosages of metronidazole (not likely at the dosage of 500mg once or twice a day in a mastiff) can cause slowing of the heart rate and that might make the slow heart rate associated with Addison's disease worse.
It is not possible at this point to really tell you if Addison's disease contributed to your mastiff's death but it does seem like it could have. On the other hand, prompt treatment for the high body temperature, along with intravenous fluid therapy, might have corrected both problems sufficiently enough to allow your dog to live through the crisis. Whether that would have actually helped enough is not certain, but it is definitely possible.
It is really hard to find yourself dealing with the loss of a pet when the loss seems unnecessary or partially due to human error, but we really are all susceptible to making bad judgments and once that process starts it seems to just induce further bad judgments in a vicious cycle, in some cases. Hopefully, the folks at the kennel will learn from this experience and use the information to prevent a future occurrence, someday --- or at least to get treatment promptly if they see these signs again.
It is very helpful if you spell out what you want done in an emergency with any kennel you may deal with in the future. It also helps to figure out transportation plans for a pet to get from the kennel to the veterinary hospital, when necessary. Having a friend who is willing to be "on call" can really help. Getting directions from your vet for what to do after hours and on weekends or holidays is important, too. If the kennel ever needs to take a pet to the emergency clinic, or make arrangements for the pet to get there, it can help a lot if it is clear that you want them to do that and if you have left a deposit to go towards emergency veterinary care, if you have reason to suspect it might be necessary.
I hope that this information is helpful to you. It is so hard when a young pet dies unexpectedly, especially when it wasn't possible to be with them to make all the decisions that had to be made.
Mike Richards, DVM
Addison's disease (Hypoadrenocorticism)
Addison's disease is also known as hypoadrenocorticism. It is an insufficient production of adrenal hormones by the adrenal gland. Since these hormones are essential for life, this is an extremely serious disease and it must be treated as such.
Adrenal insufficiency can be primary or secondary. Primary adrenocorticism affects salt/potassium balance in the body and glucorticoid as well. Secondary adrenocorticism usually only affects the glucocorticoids. It is not known why primary adrenocorticism occurs but it may be an immune mediated process. Secondary adrenocorticism probably occurs most often when prednisone or other cortisone being administered for medical reasons are suddenly withdrawn. It can occur as a result of pituitary cancer or some other process that interferes with production of hormones that stimulate the adrenal glands.
Most dogs with Addison's disease initially have gastrointestinal disturbances like vomiting. Lethargy it also a common early sign. Poor appetite can occur as well. These are pretty vague signs and it is extremely easy to miss this disease. More severe signs occur when a dog with hypoadrenocorticism is stressed or when potassium levels get high enough to interfere with heart function. Dogs with this problem will sometimes suffer severe shock symptoms when stressed, which can lead to a rapid death. When potassium levels get high heart arrythmias occur or even heart stoppage which also is fatal. In some cases, especially secondary Addison's disease, there are no detectable electrolyte changes.
This disease can be picked up by changes in the ratio between sodium or potassium by accident at times. When this happens it is still extremely important to treat for it. It is confirmed by an ACTH response test -- administration of this hormone should stimulate production of adrenal hormones. If this does not occur then hypoadrenocorticism is present. In cases in which the electrolyte levels are normal this is the only test for the problem and it will be missed unless it is looked for specifically. At times this disease can be hard to differentiate from renal failure because the symptoms and even the bloodwork can be similar ---- so the ACTH response test may be necessary to differentiate them.
Treatment for this disease is usually done by oral administration of fludrocortisone acetate (Flurinaf), salting the food, and administration of corticosteroids like prednisone. In a crisis situation this disorder must be treated more aggressively with intravenous fluids, IV glucocorticoids and correction of acid/base balances.
You have to pay close attention to a dog with this problem. Don't ignore any changes in appetite, GI disturbances or anything else that makes you think your dog is ill. If you work with your vet and are careful about following his or her directions this disease has a good prognosis when it is discovered before a crisis occurs.
Mike Richards, DVM
Kidney problems from Cushing's treatment, Addisonian state
In early Oct. my 141/2 yr. old neutered male doxie was diagnosed w/Cushing's Disease. He had all the customary testing i.e. Dex suppression tests etc. and the test indicated Pituitary Dependent Cushing's. The vet elected to start him on Lysodren.
He was admitted after finishing a 5 day course of this drug with vomiting and increased diarrhea-he also has colitis and hypothyroidism so some diarrhea was normal- but this was worse. The vet kept him on fluid therapy for 2 days before doing labs. On the second day he ordered a chem panel and found that his "kidney's were failing". This suprised me as his Bun was only slightly elevated before initiation of Lysodren therapy and his Creatinine had been normal.
He kept him on fluid for another 48 hrs and his kidney values improved only slightly-BUN down to 112. He was discharged to my care on a low protein diet and PO4 binders.
We repeated labs a week later and BUN was up to 128 and urine tests showed he wasn't concentrating his urine. I was told that Darcy was entering ESRD and that the prognosis was not good.
My vet was opposed to giving subq fluid but as I work in a hospital and have access to the equipment and had friends with training help I started giving him 200ccs of fluid every other day. In addition, I started him on 5mgs of Pepcid in the morning.
Initially he was very weak, thin and had lost a great deal of muscle. Very soon his appetite improved, he gained wt and got stronger. He went from 14.25lbs to 16lbs now.
He's had labs repeated and on 11/1 is BUN was 128, 11/19 BUN was 56, 11/19 BUN was 56, 11/26 BUN was 57, 12/2 BUN was 59 and Creatinine was 1.7. His last labs were done on 12/30 and showed a BUN of 21 and a Creatinine of 1.2. Darcy did have a bout of pneumonia in November due, I believe, to aspiration of the liquid aluminum hydroxide I was giving him by syringe. He responded well to the antibiotics and his WBCs were normal on his last CBC. I have since found an aluminum hydroxide product in tablet form so I no longer risk using the liquid.
I should also add that Darcy was started on Epogen because of low PCV. This has improved enough so that I have cut way back on the Epogen for fear of increasing his PCV too much too fast.
My questions are:
When should I next have him tested? My vet is sometimes reluctant to do labs -and I don't need unnecessary expense-taking the leave well enough alone approach but Darcy's made such good progress I don't want to let anything realistically treatable slide. What is a responsible schedule for testing and rechecks while all is going well?
Is it possible that his kidney's were so "insulted" by the Lysodren that they failed but by so aggressively supporting them we've allowed them to recover? Could it be that this is not primary kidney disease after all and that if I get him through this he will no longer have kidney disease? I've read that kidney disease is not reversible and is always progressive. What could account for the improvement in his lab values?
What do I do about the Cushing's Disease? We've all but forgotten about that during the this time and I certainly don't want to put him thru any more Dex tests. Would Anipryl be risky? His hair has almost all come back since the Cushing's diagnosis and his water consumption and peeing are normal when you consider the subq fluid. He used to get me up 3-4 times per night to drink and pee and now usually sleeps thru the nite.
He's started itching lately. I know there are may possible causes but do you have any suggestions? The vet prescribed Atarax but that caused agitation and disorientation and I stopped it. He's on so many meds that I don't know how to distinguish between and allergic rxn and a skin disease. I don't see anything abnormal but there are some rough spots on his chest. I've read about a condition called calcinosis cutis-Darcy takes calcium carbonate on an alternating basis w/ the aluminum hydroxide as PO4 binders-could that be the cause? If it is ,is the condition dangerous?
Sorry for going on so long but I love this dog alot and have worked very hard to get him through this. I'm afraid I'll overlook something simple. I know he won't live forever but I do want him to have as much quality time as possible. Other than these recent catastrophes, he's been doing remarkably well and enjoying his life.
Thanks for your help. Donna
I think that there is a good chance that the kidney problems were due to the treatment for Cushing's disease. Approximately 5% of dogs treated with mitotane (Lysodren Rx) develop side effects consistent with hypoadrenocorticism (Addison's disease). This requires supplementation with either glucocorticoids or mineralocorticoid medications to prevent adverse effects, including kidney failure. If there was an Addisonian state induced by the use of mitotane there would be a good chance of recovery with fluid therapy and time, as the damage to the kidneys tends to fall more into the "one time insult" category rather than into a chronic progressive kidney disease category. As the adrenal glands recover from the effects of Lysodren over time, they will produce corticosteroids again in most, but not all, dogs. When this happens you will see the same signs that were present previously, such as increased drinking, increased urination, hair loss, thinning of the skin, muscular weakness, etc. It would be necessary to consider treatment again at that time. There is some chance that the current itchiness is due to calcinosis cutis, a secondary effect of Cushing's disease, but it would be good to rule out a secondary bacterial infection since there was a period when it is likely that your doxie's immune system wasn't working very well. If there was no response to antibiotics it may be necessary to think about administering corticosteroids. This seems really odd to think about in a patient suspected of having Cushing's disease, but it is not uncommon for suppressed allergies or other conditions responsive to corticosteroids to surface after treatment for Cushing's disease. The reason is that the dog was producing high levels of corticosteroids due to the disease, which was masking other symptoms. There would likely be a time when the symptoms would be suppressed again by natural recovery of the adrenal glands.
All of the above is based on the assumption that an Addisonian state was induced by therapy for Cushing's disease. The only way to really know if that happened is to do ACTH testing to determine if there is a response to the administration of ACTH. If a baseline blood sample is drawn, then ACTH administered (stimulates the adrenal gland) and blood drawn an hour later shows no response to the hormone, then it is very likely that the Lysodren completely wiped out the ability of the adrenal gland to produce cortisol, at least temporarily.
I understand why you might not want to do testing, especially now when things have improved so much. It would be necessary to do some type of testing prior to considering starting Lysodren again. It would be possible to start selegiline (Anipryl Rx) without further testing and to monitor clinical signs rather than lab values to assess success of therapy. At the present time the best study that I can find suggests that Anipryl is very effective in about 20% of the cases of hyperadrenocorticism and moderately effective in another 20%, so you would have to accept that the odds of success are less than 50%. You can always go back to Lysodren, or elect not to treat for Cushing's disease, if desired. If you do go back to Lysodren it would be probably be best to do ACTH testing shortly after starting treatment (maybe 72 hours) and then on frequent intervals until a maintenance dosage of Lysodren could be established. In any case, doing ACTH testing at the first sign of loss of appetite or vomiting would be a good idea.
I am hopeful that Darcy has continued to show progress in the kidney values and that it has not been necessary to adminster Epogen (Rx) again. I am glad that you went ahead with fluid therapy, as it almost certainly helped in his recovery. I don't think it is necessary to continue the fluid therapy at this point if he has had another good test for kidney values (BUN < 30, Creatinine <1.5).
Mike Richards, DVM
Addison's in Dobie
Question: Our 10 year old Dobie was diagnosed at Auburn University 2 months ago with Addisons Disease. Prior to the diagnosis and treatment she dropped over 10 lbs in weight. Since that time, our local vet has done complete bloodwork every 2 weeks. Since she was at Auburn, she has gained 17 pounds (from 49 to 66). She gained 11 pounds in 1 week after she came home from Auburn, as we were feeding her canned Canine Maintenance, (4 cans a day). Aftr she gained all her weight back, we put her on Dry Canine Mainenance. She has been on Dry food for over one month. She gets a small ball of canned food each morning with her Prednisone (5 mg daily). She also gets an injection of the hormone necessary every 24 days. Her Potassium and Sodium appear to have stabilized. And more importantly, she is back to her old (very active) self. Since the beginning of the treatment the Vet has taken blood work to establish the correct dosages. However, the blood work has shown another potential problem: Her triglicerides and Lipace are extremely out of line. Her chart is:
4/27 Triglicerides 454 Lipase 822 (Not Fasted)
5/4 Triglicerides 132 Lipase 832 (Not Fasted)
5/25 Triglicerides 67 Lipase 927 (After fasting for 12 hours)
6/7 Triglicerides 2,955 Lipase 1,021 (Not Fasted)
Today we had another test performed after fasting and the blood looked normal, however, our Vet appears stumped and very concerned. He wants our Dobie to go back to Auburn for more testing. He suggess Hypo Thyroidism, Pancreatitis, and any other thing he can think of. He is trying to help, but we would like your opinion. Please help.
Fasting can make a HUGE difference in the level of triglycerides in the blood stream. Therefore, I tend to think that the triglyceride levels going up and down as they have is probably just the difference between fasting and non-fasting blood levels. However, it is reasonable to check for hypothyroidism in a 10 year old doberman since the disorder is reasonably common in this breed.
I can truly understand why your vet feels that the triglyceride levels must indicate a problem. I have been really really surprised at the difference between fasting and non-fasting samples for this particular lab value. Until you run across one of these patients it is hard to believe it could change that much just due to a meal.
The lipase levels are more confusing. Lipase levels elevate most commonly with kidney disease, dehydration affecting the kidneys and with pancreatitis. My first instinct would be to think about dehydration in a patient with Addison's disease, since patients with this disease may have subclinical dehydration when they are not quite stabilized. I do think it would be worth talking to the vets at Auburn about this possibility, or at least to report that the lipase levels are elevated.
Chronic pancreatitis is possible but it sure doesn't sound much like it is a problem with all the improvement so far.
I think you'll find that there isn't a serious problem underlying these lab values, except perhaps a small amount of need for thinking over the regulation of the Addison's disease and monitoring for kidney problems as time goes on. However, I really do think that you should check back with the vet that handled your dobe's case at Auburn, or ask your vet to do that, to discuss the increase in lipase.
Good luck with this.
Mike Richards, DVM
Hypoadrenocorticism (Addison's disease) considered in surgery for tumor
Q: dr. mike, I have written to you on several occasions about our pitbull with Cushings and her first stimulation test,etc. which was 1 and 1. They are going to do another stimulation test before giving her anything else. but this same dog has other problems as well. She has had a growth going on in her L hind leg for at least a year. Our local vet referred us to K-State for this after aspirating it in several different places and finding nothing but fat, rbc's, wbc's, etc. as she has a hx of having skin mast cell tumors. K-State also aspirated and found pretty much the same thing as our local vet. But they feel that surgery needs to be done as it just keeps getting bigger and causing her problems. My question is: Since this dog has Cushings and this disease tends to cause muscle weakness, and the heart is considered a muscle, what is your opinion of testing that should be done before she undergoes anesthesia, and so forth? Should she have an US of the heart? Or just routine EKG's? This dog will be 10 years old 10/19/99. Also the mast cells that have been removed on her has actually been once. Other growths removed were mainly of some other consistency. Also what should her ACTH stimulation tests run before she undergoes surgery? If her stimulation test that she will have done tomorrow does not come back any higher, or lower than the first one ( 1 and 1), will it be safe to go ahead with this surgery on her leg?
thank you for your time, R.
A: R I am very uncomfortable doing surgery on a dog with hypoadrenocorticism (Addison's disease), which I think is the current state that your pitbull is in, based on the lab tests. Surgery is a stress and hypoadrenocorticism reduces the body's ability to handle stress. So I would tend to be very cautious about going ahead with surgery prior to fully understanding the hormonal status. Hopefully the most recent ACTH stimulation test will help to clear up that issue. If her heart sounds normal and she has a normal ECG it is probably not necessary to do cardiac ultrasound exam but if it makes you more secure to have it done there isn't a reason not to do it, either. It is important to have a lab panel with electrolyte levels prior to surgery in a patient who may have hypoadrenocorticism. It is necessary to place an IV catheter and run saline solution during the surgery as this helps to keep potassium levels normal, which is important in patients with hypoadrenocorticism. It may be necessary to supplement glucocorticoids post-surgically to keep them in a physiologically normal range during the time of stress but the vet school will be advising you on the necessity of this, I'm sure.
If there isn't an immediate pressing need to remove the tumor I really think it is important to discuss with your vets the ramifications of the current lab work and to discuss whether it might be better to put surgery off until there is a more normal response on the ACTH stimulation test.
It is important to eventually rule out the possibility of a return of mast cell tumors, too. So when there is a clear understanding of whether or not your dog will have to be treated as a patient with hypoadrenocorticism or not, it would be best to proceed. More caution will be necessary if hypoadrenocorticism persists but you will at least be aware of this need. A normal ACTH stimulation test has a pre, or baseline, value of 0.5 to 4.0 ug/dl and a post ACTH stimulation value of 8.0 to 20 ug/dl. In patients in which hyperadrenocorticism is being well controlled, most vets look for values for the prestimulation sample of less than 4 ug/dl but more than 1 ug/dl and post ACTH values of 1 ug/dl but less than 5 ug/dl.
So the "1 and 1" value is technically right on the borderline of what is desired but without any rise in the value is suspicious of adrenal tissue destruction of a greater magnitude than usually occurs with initial dosages of Lysodren. Most dogs with this problem will get more normal values within a few weeks but some dogs continue to have low values for months. It is necessary to do periodic testing to determine what the levels are as long as they continue to stay so low, without any rise in response to ACTH stimulation.
I would want to wait at least a few weeks for more normal results before deciding on the surgery.
Mike Richards, DVM
Addison's and Florinaf
Q: Dear Dr. Mike; First of all, I'd like to thank you for being there for us ! Your information has helped us tremendous in the illness of our beloved Cardigan Corgi. She nearly died before being diagnosed as suffering from Addison's disease, and altho our Vet is a fine compassionate ,young doctor and correctly diagnosed our Dylan, the extensive information about the disease I found at your marvellous Web site!! Our Dylan was put on Florinef Acetate,0.1 mg tabs, one of these 3 times daily, together with 1 Prednisone tablet in the morning, this seems to be a large number of drugs to us to give her every day! Our Dylan has just turned 3 years old and we hope that you can answer our concern, is this disease a lifetime, chronic disease or will she ultimately be cured of this? The medicine (Florinef Acetate) is most expensive and cost $ 50.00 for 100 tabs, however altho my wife and I live on Social Security, we would gladly cut down on our food to keep this little Angel alive!! We cannot purchase this medicine from our Vet, except for the Prednisone and wonder if there is perhaps a less expensive source for the Florinef, other than the local drug store? Any help you can give us is greatly appreciated, Dr. Mike and THANK YOU for being there and for the obvious GREAT compassion you show for the animals!
A: H. - I am not aware of a generic equivalent of Florinef (Rx). It will almost certainly be necessary to keep Dylan on this medication lifelong and in many instances it is necessary to increase the dosage as time goes on. I do not follow the mail-order medication market for veterinary medicine very closely but have not seen this medication for sale in the times I have looked at these publications. You may want to ask your vet about ordering the Florinef for you. I am pretty sure that The Butler Company, a veterinary distributor, carries Florinef. Sometimes, but not always, it is possible for a veterinarian to sell a medication for less than the pharmacy and still make enough profit to justify ordering the medication. That is one of the good things about being a veterinarian - we're mostly independent small businessmen who can choose to make a little less in some cases if we want to. Pharmacists working for the larger corporations might not have this option. It is worth explaining the need for a lower cost source of Florinef to your vet to see if such an arrangement can be worked out.
Mike Richards, DVM
Addison's treatment and pain control
Q: Dr. Mike. I desperately need your advice since my dog is in a lot of pain and my vet seems to be running out of solutions. I adopted my dog 4 yrs. ago from the shelter and I think my dog may be around 12 yrs. old. He is a Shih -Tzus with very bowed front legs and weighs 16 lbs. About a month ago my dog started having a hard time getting up in the morning because of pain in his hips . I treated him with asprin for a week and his condition improved . My vet x-rayed his back legs and discovered my dog had knee joints which protrubed out of the sockets and had very bad hip dysplasia . He prescribed Rimadyl and his condition improved. When my dog was on either asprin or Rimadyl he was able to walk and was peppy most of the time. A week ago my vet discovered from blood tests (ACTH response test) that my dog had Addison's disease. He prescibed FLORINEF (0.1 MG twice daily) and Prednisolone (5 mg per day ). The Rimadyl was discontinued and this is when the problem got worse. He has been on the Florinef and Prednisolone and now he can barely walk and is very weak and doesn't want to move. Also he had diarrhea today. Two days ago in addition to the Florinef and Prednisolone my vet also gave my dog his first shot of Adequan and an anti-inflammatory injection and put him on a dextrose IV for a few hours. Two days later after these injections and IV, my dog seemed to have taken a turn for the worse and my vet is out of answers. In my view, my dog seem to take a turn for the worse once the Rimadyl was discontinued and the treatment for Addison's disease started. Now my dog does not want to get out of his bed and he seems to be in a lot of pain. Please help me. Could the results from the ACTH test be wrong? Is the Prednisolone helping with the hip dysplasia and does it work as effectively as Rimadyl? What else can my dog be prescribed for the pain in his hips in light of the Addison's disease? I was told that my dog cannot take asprin or Rimadyl with the Florinef and Prednisolone. Please help my dog is very sick and I am running out of solutions. Up until today my dog has been eating ok and has been drinking water, but I have to carry him outside to go to the bathroom and he cannot walk very well. My vet does not want to put him to sleep because he thinks there may be some hope. Thank you for any advice you may have.
A: JCJC- To the best of my knowledge there is no reason not to use aspirin or carprofen (Rimadyl Rx) in conjunction with fludrocortisone acetate (Florinef Rx). However, there is reason to believe that concurrent administration of glucocorticoids such as prednisone and non-steroidal anti-inflammatory medications (NSAIDS) such as aspirin or Rimadyl does increase the chance of gastrointestinal effects including ulceration. For this reason, most vets are reluctant to use these medications together. There is an FDA approved medication that is a combination of aspirin and methylprednisilone, though, called Cortaba (Rx). I always thought it was odd that there were warning against using these products together and an approved medication containing both.
In desperate situations it is worth considering desperate measures and I don't think I'd be afraid to use Rimadyl with the other medications, especially since it is less likely to have GI effects than other NSAIDS. The manufacturer of Rimadyl, Pfizer, recommends against this combination at the current time if you want a third opinion.
I think sometimes lab tests are in error. The clinical signs you mention could be seen with Addison's disease, though. In most cases it is a good idea to rerun the tests to gauge the effects of the medications so your vet may have already done this. If the results were surprising it may be that there is a need to rethink this diagnosis but the only way to tell is to check.
Addison hund

Addisons sjukdom
Binjurebarken har normalt som uppgift att utsöndra livsnödvändiga hormoner. Av dessa hormoner är kortisol bland de viktigaste då det hjälper till att balansera kroppen i stressituationer genom att reglera blodtryck och hjärtfrekvens. Om sjukdomen går obehandlad under en längre tid kan hunden drabbas av en ”Addison-kris” som är en livshotande stadium där blodcirkulationen sviktar och återförseln av blod till hjärtat är otillräcklig. Hundar som har Addisons sjukdom uppvisar diffusa symtom som allmän trötthet, muskelsvaghet, diarrèe, ökad törst och aptitlöshet. Diagnosen ställs genom ett s.k. ACTH test där man stimulerar hormonutsöndringen från binjurebarken och sedan mäter koncentrationen kortisol i blodet före och efter stimulering.
Både produktionen av kortisol och aldosteron är utslagen.
Bara produktionen av kortisol är utslagen, hunden kan fortfarande producera aldosteron. Kan utvecklas till primär addison med tiden.
Background
My name is Glenn Kardel. I have polyglandular autoimmune syndrome type II, frequently referred to as Schmidt's syndrome. The classic manifestations of this syndrome are adrenal insufficiency plus autoimmune thyroid disease and/or insulin dependent diabetes mellitus. I have all three of the above conditions: Addison's disease, hypothyroidism, and type I diabetes.
The goals of this site are:
- Provide information about Addison's disease, type I diabetes, and the interaction between the two conditions.
- Share the techniques I've used to control my diabetes in the face of the added pressure of Addisons.
- Provide an opportunity for others to share information, experiences, and advice on Addison's disease and diabetes.
Please consult your physician before implementing any of the
Addison hund
 Hvad er Addisons?
Hvad er Addisons?
Addisons Sygdom eller Hypoadrenocorticisme er en tilstand, hvor kroppen ikke danner tilstrækkeligt med binyrebarkhormon.
Binyrerne er organer, der sidder i bughulen. En binyre består af to lag: barken (cortex) og marven (medulla).
Barken danner hormonerne cortisol (glucocorticoid) og aldosteron (mineralocorticoid).
Marven danner hormonet adrenalin, der IKKE påvirkes af Addisons Sygdom.
Cortisol kaldes også for stresshormonet. Kroppen udskiller det til blodet i øgede mængder ved stresstilstande som f.eks. sygdom eller angst.
Der er 2 forskellige former for Addisons Sygdom:
- Primær Addisons: opstår almindeligvis på grund af en autoimmun reaktion i binyrerne.
- Sekundær Addisons: opstår på grund af forstyrrelser i hypofysens (del af hjernen også kaldet “koglekirtlen”) udskillelse af et regulerende hormon, der styrer binyrernes dannelse af hormoner.
Symptomerne på Addisons
Sygdommen kan optræde i mange forklædninger. Sygdommen ses ofte hos den yngre hund. Ejer beskriver ofte en hund, der virker sløv og som har “mistet glansen i øjnene”.
Den bliver let udmattet, mangler appetit og kan have vekslende afføring. Opkast kan forekomme on/off.
Rysteture og skælven er også almindelig symptomer, der kan lede tankerne hen på Addisons.
I nogle tilfælde kommer hunden til klinikken og er fuldstændig “flad”.
Symptomerne kan komme og gå.
I perioder kan hunden være frisk, hvilket kan gøre det svært at få mistanken om Addissons, da mange andre sygdomme kan give lignende symptomer.
Hvordan stilles  diagnosen?
diagnosen?
Ofte vil det være en general blodprøve, der kan lede mistanken mod Addissons. Saltbalancen i blodet vil ofte være skæv, hvis en hund har Addissons. Saltene består blandt andet af elektrolytterne chlorid, natrium og kalium. Er chlorid lav, kalium høj og natrium lavt, vil det være en indikator for Addisons. Man sammenholder disse to tal (natrium/kalium ratio), og hvis den groft set er under 25, er der en ubalance. Blodet vil ofte også vise et højt antal af lymfocytter, forhøjede leverværdier og nyreværdier samt blodmangel.
Det er dog IKKE ALTID, man ser disse forandringer i blodet hos en Addisons patient.
Den endelige diagnose stilles ved en “ACTH-stimulationstest”:
- Dyrlægen udtager en blodprøve, hvor mængden af cortisol i blodet måles (0-prøve).
- Derefter gives en injektion med et stof (synachten), der giver besked til binyrerne om at producere cortisol.
- En time efter udtages endnu en blodprøve, hvor man igen måler mængden af cortisol i blodet.
Hvis der ikke er dannet tilstrækkeligt med cortisol, kan diagnosen Addisons med rimelighed stilles. Det vil altid være en individuel vurdering fra dyrlægen vurdering, der danner grundlag for diagnosen, da alle patienter er forskellige og mange ting skal tages i betragtning.
Hvordan behandles Addisons Sygdom?
Hunden skal have tilført binyrebarkhormon i pilleform.
Man giver to forskellige slags hormoner: Prednisolon og Florinef.
Over nogle måneder vil dosis af Prednisolon ideelt set kunne mindskes.
Nogle hunde vil på sigt slet ikke have brug for Prednisolon til hverdag, men kun i tilfælde af stresstilstande.
Efter opstart af behandlingen skal der efter 1-2 uger tages en blodprøve. Man bruger natrium/ kalium forholdet som pejlemærke for korrekt dosering.
Man skal derfor ikke lave en ny ACTH-stimulationstest hver gang man skal vurdere, om hunden er korrekt medicineret.
Det er naturligvis altid vigtigt at se på hundens tilstand: hvordan har den det? Det skal altid sammenholdes med blodprøvesvar, herefter er det dyrlægens fortolkning sammen med ejerens observationer, der bestemmer medicindosis.
I nogle tilfælde kan hundens værdier ved stimulationstesten ligge i et “grænseområde”. Hvis der er indikationer nok på sygdommen, kan man give dyrene en behandling med en lav dosis af hormoner og herefter vurdere effekten.
Addisons er en meget kompleks sygdom, hvor svarene ikke altid er ” sorte og hvide”. Hvis hunden ingen hormoner danner overhovedet er det mere simpelt at gå til behandlingen. Hvis hundens tal er “lige på grænsen”, er det mere kompleks. Måske derfor sygdommen ofte undervurderes?
I USA er det almindeligt, man bruger man en anden behandlingsmetode, der endnu ikke er så udbredt i Danmark. Man giver som alternativ til florinef en indsprøjtning med et stof, der hedder Percorten-V. Princippet i medicinen er, at hormonerstatningen frigives langsomt over en lille måneds tid. Efter injektionen måler man blodets indhold af elektrolytter, og lader det være pejlemærke for hvornår næste indsprøjtning skal gives, samt hvor stor dosis af Prednisolon, der skal suppleres med. I Danmark kan produktet kun fås, hvis dyrlægen får en særlig udleveringstilladelse.
Fremtidsudsigterne for en hund med Addisons?
En hund med Addisons kan få et langt godt liv. Det stiller naturligvis krav til ejeren om, man skal være omhyggelig med at give medicinen hver dag. Man skal også være indstillet på indimellem at skulle til dyrlægen og få hunden tjekket ved f.eks. en blodprøve.
Addisons kan både betragtes som en overset og en underestimeret sygdom.
Diagnostikken og behandling stiller krav til både ejer og dyrlæger. Med det rigtige veterinære arbejde og kærlighed til dyrene, kan Addisons hunde få et værdigt og godt liv!
Kan en sygdom behandles indenfor rimelighedens grænser, så man ikke går på kompromis med etik og livskvalitet for dyrene, fortjener alle liv at have liv!
Af Dyrlæge Lise Rovsing
Følg Dyrlæge Lise Rovsings Blog her!
Mangler du pasning af dit kæledyr?
Et pasningsnetværk i regi af Artemis' klienter - for kolde snuder og varme hjerter.
Følg os på facebook i gruppen "Dyreklinikken Artemis' venner"
Kom med til hundetræning - hvalpekursus
Har du fået hvalp eller står overfor at skulle havde det?
BETALING
Afregning ved hvert besøg!
ARTEMIS DYREKLINIK • GERSONSVEJ 2 • 2900 HELLERUP
Комментариев нет:
Отправить комментарий